Dementia Risk Rises If You Live With Chronic Pain, Study Says
People with multiple sites of body pain performed worse than people with no pain on seven of 11 cognitive tasks, the study found.Sunday, January 28th 2024, 9:15 am
Chronic pain, such as arthritis, cancer or back pain, lasting for over three months, raises the risk of cognitive decline and dementia, a new study found.
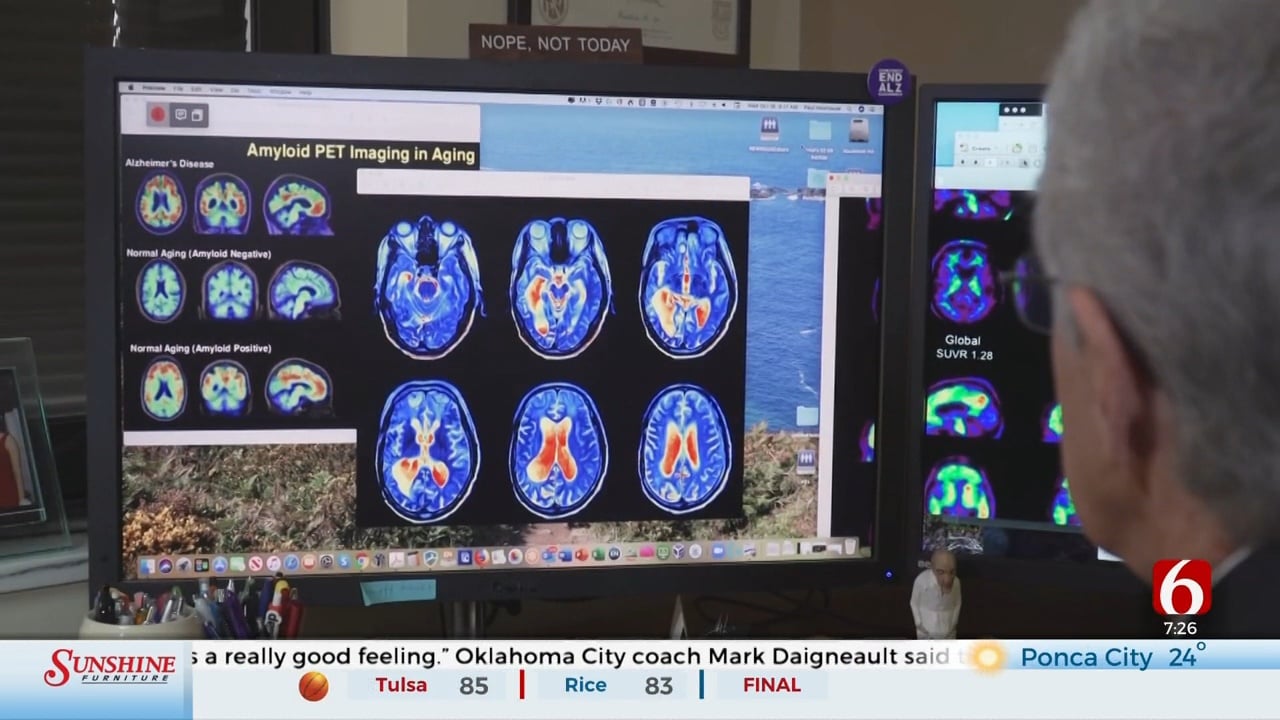
The hippocampus, a brain structure highly associated with learning and memory, aged by about a year in a 60-year-old person who had one site of chronic pain compared with people with no pain.
When pain was felt in two places in the body, the hippocampus shrank even more — the equivalent of just over two years of aging, according to estimates in the study published in the journal Proceedings of the National Academy of Sciences, or PNAS.
"In other words, the hippocampal (grey matter volume) in a 60-y-old individual with (chronic pain) at two body sites was similar to the volume of (pain free) controls aged 62-y-old," wrote corresponding author Tu Yiheng and his colleagues. Tu is a professor of psychology at the Chinese Academy of Sciences in Beijing.
The risk rose as the number of pain sites in the body increased, the study found. Hippocampal volume was nearly four times smaller in people with pain in five or more body sites compared with those with only two — the equivalent of up to eight years of aging.
"Asking people about any chronic pain conditions, and advocating for their care by a pain specialist, may be a modifiable risk factor against cognitive decline that we can proactively address," said Alzheimer's disease researcher Dr. Richard Isaacson, a preventive neurologist at the Institute for Neurodegenerative Diseases of Florida. He was not involved in the new study.
Cognition declined with pain
The study analyzed data from over 19,000 people who had undergone brain scans as part of the UK Biobank, a long-term government study of over 500,000 UK participants between the ages of 40 and 69.
People with multiple sites of body pain performed worse than people with no pain on seven of 11 cognitive tasks, the study found. In contrast, people with only one pain site performed worse on only one cognitive task — the ability to remember to perform a task in the future.
The study controlled for a variety of contributing conditions — age, alcohol use, body mass, ethnicity, genetics, history of cancer, diabetes, vascular or heart problems, medications, psychiatric symptoms and smoking status, to name a few. However, the study did not control for levels of exercise, Isaacson said.
"Exercise is the #1 most powerful tool in the fight against cognitive decline and dementia," he said via email. "People affected by multisite chronic pain may be less able to adhere to regular physical activity as one potential mechanism for increased dementia risk."
Equally important is a link between chronic pain and inflammation, Isaacson said. A 2019 review of studies found pain triggers immune cells called microglia to create neuroinflammation that may lead to changes in brain connectivity and function.
People with higher levels of pain were also more likely to have reduced gray matter in other brain areas that impact cognition, such as the prefrontal cortex and frontal lobe — the same areas attacked by Alzhemier's disease. In fact, over 45% of Alzheimer's patients live with chronic pain, according to a 2016 study cited by the review.
The study was also not able to determine sleep deficits — chronic pain often makes getting a good night's sleep difficult. A 2021 study found sleeping less than six hours a night in midlife raises the risk of dementia by 30%.
A global disability
Globally, low back pain is a leading cause of years lived with disability, with neck pain coming in at No. 4, according to the 2016 Global Burden of Disease Study. Arthritis, nerve damage, pain from cancer and injuries are other leading causes.
Researchers estimate over 30% of people worldwide suffer with chronic pain: "Pain is the most common reason people seek health care and the leading cause of disability in the world," according to articles published in the journal The Lancet in 2021.
In the United States alone, at least 1 in 5 people, or some 50 million Americans, live with long-lasting pain, according to the US Centers for Disease Control and Prevention.
Nearly 11 million Americans suffer from high-impact chronic pain, defined as pain lasting over three months that's "accompanied by at least one major activity restriction, such as being unable to work outside the home, go to school, or do household chores," according to the National Center for Complementary and Integrative Health.
Chronic pain has been linked to anxiety, depression, restrictions in mobility and daily activities, dependence on opioids, increased health care costs, and poor quality of life. A 2019 study estimated about 5 million to 8 million Americans were using opioids to manage chronic pain.
Treating chronic pain
Pain management programs typically involve a number of specialists to find the best relief for symptoms while providing support for the emotional and mental burden of pain, according to John Hopkins Medicine.
Medical treatment can include over-the-counter and prescription medications to stop the pain cycle and ease inflammation. Injections of steroids may also help. Antidepressants increase the amount of serotonin, which controls part of the pain pathway in the brain. Applying brief bursts of electricity to the muscles and nerve endings is another treatment.
Therapies such as massage and whirlpool immersion and exercises may be suggested by occupational and physical therapists. Hot and cold treatments and acupuncture may help as well.
Psychologists who specialize in rehabilitation may recommend cognitive and relaxation techniques such as meditation, tai chi and yoga that can take the mind off fixating on pain. Cognitive behavioral therapy is a key psychological treatment for pain.
Going on an anti-inflammatory diet may be suggested, such as cutting back on trans fats, sugars and other processed foods. Weight loss may be helpful as well, especially for back and knee pain, according to Johns Hopkins.
More Like This
January 28th, 2024
November 25th, 2024
November 21st, 2024
November 14th, 2024
Top Headlines
December 14th, 2024
December 14th, 2024
December 14th, 2024
December 14th, 2024